The 2 main classifications of lung cancer are small cell lung cancer (SCLC) and non-small cell lung cancer (NSCLC).
Based on results from the National Lung Screening Trial, lung cancer screening is done with a test called a low-dose CT lung scan. Yearly scan is recommended for people aged 55 to 74 who have smoked for 30 pack years or more or who have quit within the past 15 years.
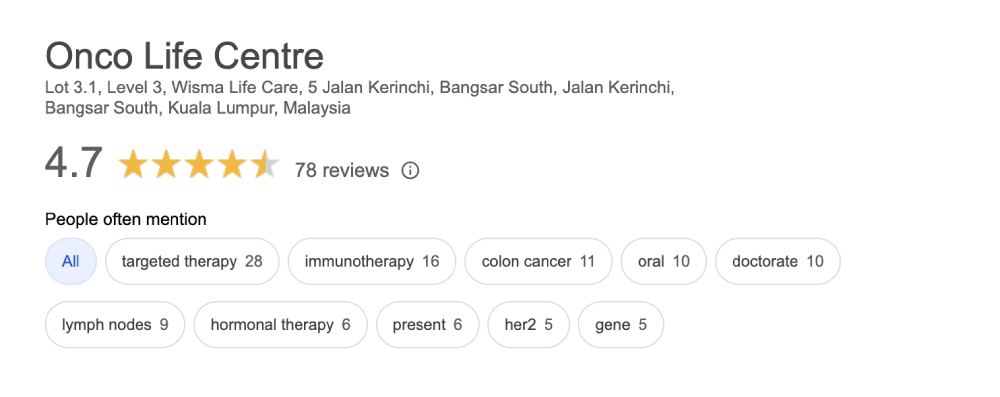
Talk to our highly experienced oncologists at Onco Life Centre about your lung cancer treatment options. Treatment recommendations by our lung cancer specialists at Onco Life Centre are tailored and personalized according to the latest NCCN and FDA guidelines. Lung cancer treatment options also depend on the type and stage of lung cancer, genetic changes in the tumor, and the patient’s preferences and overall health. The landscape of drug treatment in NSCLC has evolved immensely over the last 5 years.
The goal of surgery is complete removal of the lung tumor and the nearby lymph nodes in the chest.
The types of surgery used for NSCLC include lobectomy, wedge resection, segmentectomy and pneumonectomy.
Adjuvant chemotherapy for non small cell lung cancer is given after surgery to lower the risk of the lung cancer returning. It is intended to get rid of any lung cancer cells that may still be in the body after surgery.
The most common type of radiotherapy for lung cancer is called external-beam radiation therapy. A radiation therapy regimen usually consists of a specific number of treatments given over a set period of time. CT scans may be used to plan out exactly where to direct the radiation to lower the risk of damaging healthy parts of the body. This is called intensity modulated radiation therapy (IMRT) or stereotactic body radiation therapy (SBRT).
Chemotherapy stops the cancer cells’ ability to grow and divide. Chemotherapy improves both the length and quality of life for people with lung cancer of all stages. Chemo for non small cell lung cancer is usually given through a vein as an intravenous (IV) infusion. The type of lung cancer you have, such as adenocarcinoma or squamous cell carcinoma, affects which drugs are used for chemotherapy. Side effects of new and modern drugs are well managed by our lung cancer specialists.
Lung cancer targeted therapy targets the cancer’s specific genes, proteins, or the tissue environment that contributes to cancer growth and survival. To find the most effective treatment, our oncologist may run tests to identify the genes, proteins, and other factors in your tumor.Read More ...
Immunotherapy is designed to boost your body's natural defences to fight the cancer. The PD-1 pathway is critical in the immune system’s ability to control cancer growth. PD-1 and PD-L1 antibodies block this pathway and can stop the growth of NSCLC. The FDA has approved two immunotherapy drugs for use in metastatic non small cell lung cancer (NSCLC).
In general, stage I and II NSCLC are treated with surgery. Some patients with large tumors or signs that the tumor has spread to the lymph nodes may benefit from chemotherapy. Chemotherapy may be given before surgery (neo-adjuvant chemotherapy) or after surgery (adjuvant chemotherapy) to reduce the chance the cancer will return.
Treatment options depend on the size and location of the tumor and the lymph nodes that are involved. A combination of chemotherapy and radiation therapy is usually recommended. Surgery may be an option after initial chemotherapy or chemotherapy with radiation therapy.
Patients with stage IV NSCLC (metastatic lung cancer) typically do not receive surgery or radiation therapy. The goals of systemic therapy are to shrink the cancer, relieve discomfort caused by the cancer, prevent the cancer from spreading further, and lengthen a patient’s life. Treatment often continues as long as it is controlling the cancer’s growth.
1) First line systemic therapy for stage 4 or metastatic lung cancer depends on the genetic changes found in the tumor. For patients with tumors that have a genetic change on the EGFR, ALK, ROS1 or NTRK genes, targeted therapies called Tyrosine Kinase Inhibitors (TKI) are the preferred first-line systemic options.
For stage 4 lung cancer patients with tumors without these genetic changes in the tumor, the treatment options are based on the immunohistochemistry of the lung cancer tumor and on the intensity of PDL1 expression.
For patients with non-squamous cell carcinoma with high PD-L1 expression, immunotherapy alone, or chemo with immunotherapy and anti-angiogenesis therapy maybe recommended.
For patients with squamous cell carcinoma with high PD-L1 expression, immunotherapy-alone or combined with chemotherapy maybe recommended.
2) Second line treatment and beyond for stage 4 or metastatic lung cancer depends on the gene mutations found in the tumor and the treatments which patients have already received.
For patients with tumors that do not have a genetic change on the EGFR, ALK, ROS1 or NTRK genes and have received chemotherapy for first-line treatment, immunotherapy can be the next line of treatment if their tumors express a high level of PD-L1.
For patients with tumors that have an EGFR gene mutation, the best treatment option depends on whether the cancer has developed a mutation called T790M, which makes it resistant to the TKI. For patients with tumors that have an ALK, ROS1, BRAF gene mutation, our lung cancer specialist will help you plan your subsequent lines of treatment, which includes new generation TKIs and immunotherapy.
3) Palliative care will also be important to help relieve symptoms and side effects. Radiation therapy or surgery may also be used to treat metastases that are causing pain or other symptoms. Bone metastases that weaken major bones can be treated with surgery, and the bones can be reinforced using metal implants.
Onco Life Centre combines key elements of lung cancer care and lung cancer treatment under one roof, with convenience and speed. At Onco Life Centre, we have the necessary medical disciplines to achieve this. Our board certified highly experienced consultant oncologists have earned recognition for excellence in the field of lung cancer treatment, providing our patients with the most advanced lung cancer treatment options.

Dr. Christina Ng is a Consultant Medical Oncologist and Founder President of Empowered, The Cancer Advocacy Society of Malaysia.…
Treatment cost for lung cancer depends on several factors, such as the staging and also the sub-type of the lung cancer. Generally, using only chemotherapy is cheaper compared to using targeted therapy or immunotherapy. The more advanced the cancer stage, the more expensive it becomes to treat the cancer. At Onco Life Centre, the cost for treating lung cancer using chemotherapy for most of our patients range from MYR5,000 to MYR8,000 per cycle. Using Targeted Therapy can range from MYR6,000 and above, depending on the specific type of targeted therapy drug used. Immunotherapy can range from MYR9,000 and above depending on the specific type and dosage of immunotherapy drug used.
Patients and their families have opportunities to talk about the way they are feeling with our oncologists, nurses, counselors, or join our psychosocial program and support group at Onco Life Centre.