Cancer begins when healthy cells change and grow out of control, forming a mass called a tumor.
A cancerous tumor is malignant, meaning it can grow and spread to other parts of the body. Cancer that begins in the liver is known as primary liver cancer.




There are a number of types of primary liver cancer that occur in adults.
Patients with HCC may experience no symptoms, particularly when the tumor is detected early as part of a screening program. When symptoms or signs do occur, they include:
Some symptoms experienced by people with HCC may be caused by cirrhosis rather than the tumor.
Blood tests
AFP levels in the blood are elevated in about 50% to 70% of people who have HCC.
Computed tomography (CT) scans
HCC can be diagnosed based on features specific to liver cancer that are seen on a CT scan.
Magnetic resonance imaging (MRI)
An MRI scan uses magnetic fields to produce detailed images of the body.
Biopsy
A biopsy is the removal of a small amount of tissue for examination under a microscope.
When the AFP blood test, CT scan, or MRI strongly indicates HCC, and other test results that are typical of HCC, a biopsy may not be needed.
Molecular testing of the tumor
These laboratory tests will identify specific genes, proteins, and other factors unique to liver cancer.
Results of these tests will help determine your treatment options.
The Barcelona Clinic Liver Cancer (BCLC) system categorizes HCC based on characteristics of the tumor, liver function, performance status, and cancer-related symptoms.
BCLC stage groupings include:
The tumor is smaller than 5 cm. Liver function varies, and portal vein pressure may or may not be increased.
Patients with early-stage disease may be candidates for a liver transplant, surgery, or radiofrequency ablation (RFA).
The tumor may be large or there may be multiple tumors. Regional therapies, such as trans-arterial chemoembolization maybe recommended for these patients with intermediate stage HCC.
The tumor has invaded the portal vein or spread to other parts of the body, such as the lymph nodes, lungs, and bones.
Targeted therapy or immunotherapy maybe recommended for these patients.
These treatments are recommended for early stage liver cancer. These treatments include surgery, radiofrequency ablation, percutaneous ethanol injection, and radiation therapy.
While these treatments will most likely not eliminate the cancer, they have been shown to improve symptoms, quality of life and survival.
During chemoembolization, chemotherapy drugs for liver cancer are injected into the hepatic artery, and the flow of blood through the artery is blocked for a short time so the chemotherapy stays in the tumor longer. Read More ...
Targeted therapy is drug treatment that targets the cancer’s specific genes, proteins, or the tissue environment that contributes to cancer growth and survival. This type of treatment blocks the growth and spread of cancer cells while limiting damage to healthy cells. Read More ...
Immunotherapy, also called biologic therapy, is designed to boost the body's natural defenses to fight the cancer. Read More ...
The following factors can raise a person’s risk of developing HCC.
Risk factors are cumulative and having more than 1 risk factor increases the risk of developing liver cancer.
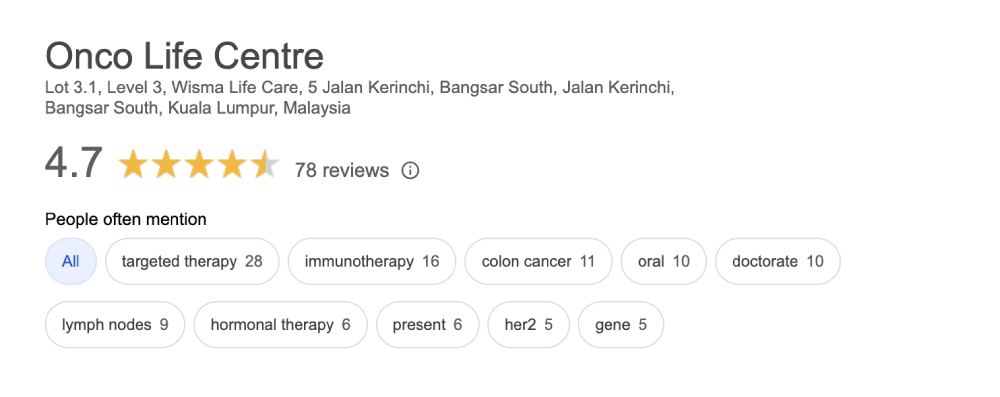
Onco Life Centre combines key elements of liver cancer care and liver cancer treatment under one roof, with convenience and speed. At Onco Life Centre, we have the necessary medical disciplines to achieve this. Our board certified highly experienced consultant oncologists have earned recognition for excellence in the field of liver cancer treatment, providing our patients with the most advanced liver cancer treatment options.

Dr. Christina Ng is a Consultant Medical Oncologist and Founder President of Empowered, The Cancer Advocacy Society of Malaysia.…
Treatment cost for liver cancer depends on several factors, such as the stage of the liver cancer. Generally, using only chemotherapy is cheaper compared to using targeted therapy or immunotherapy. The cost of liver cancer targeted therapy is from MYR4,000. Average cost of immunotherapy for liver cancer is estimated to be MYR10,000 depending on the specific type and dosage of immunotherapy drug used.
Patients and their families have opportunities to talk about the way they are feeling with our oncologists, nurses, counselors, or join our psychosocial program and support group at Onco Life Centre.