A higher risk for uterine cancers can be inherited and happens about 5% of the time. Lynch syndrome is most commonly associated with inherited uterine cancer and is also associated with colon, kidney, bladder, and ovarian cancers. Lynch syndrome is associated with DNA mismatch repair defect.
People affected by Lynch syndrome can receive increased screening for Lynch-associated cancers. Affected family members may consider preventive surgery for uterine and ovarian cancer.
In addition to a physical examination, the following tests may be used to diagnose uterine cancer.
Pap Smear is done during pelvic examination to look for abnormal glandular cells, which are caused by uterine cancer.
Endometrial biopsy allows removal of a small amount of tissue for examination under a microscope. This allows a definite diagnosis to be made.
Dilation and curettage is often done in combination with a hysteroscopy so the doctor can view the lining of the uterus during the procedure. After endometrial tissue has been removed, during a biopsy or D&C, the sample is checked for cancer cells.
Computed tomography (CT) scan allows a detailed, 3-dimensional image to exclude any abnormalities or tumors.
Magnetic resonance imaging (MRI) uses magnetic fields to produce detailed images of the body.
Doctors assign the stage of endometrial cancer using the FIGO system.
The cancer is found only in the uterus or womb, and it has not spread to other parts of the body.
The tumor has spread from the uterus to the cervix.
The cancer has spread beyond the uterus, but limited to the pelvis.
The cancer has metastasized to the rectum, bladder, and/or distant organs.
Talk to our uterine cancer oncologists at Onco Life Centre about your treatment options. The main treatments for uterine cancer are surgery, radiation therapy, chemotherapy, immunotherapy, targeted therapy and hormone therapy. Often the best approach uses 2 or more of these treatment methods. It is important that you understand the goal of your treatment. If a cure is not possible, treatment is aimed at relieving symptoms such as pain.
Hysterectomy can be simple (removal of the uterus and cervix) or radical (removal of the uterus, cervix, the upper part of the vagina, and nearby tissue). For patients who have been through menopause, the surgeon will typically also perform a bilateral salpingo-oophorectomy, which is the removal of both fallopian tubes and ovaries. Read More ...
Lymph node removal at the vicinity of the tumor will determine if the cancer has spread beyond the uterus.
Some women with uterine cancer need radiation therapy after surgery to destroy any remaining cancer cells. Read More ...
The types of systemic therapies used for uterine cancer include Chemotherapy, Hormonal therapy, Targeted therapy and Immunotherapy.
Chemotherapy for uterine cancer is aimed at destroying cancer remaining after surgery or aimed at shrinking the cancer and slowing down the tumor's growth if it recurs after initial therapy.
Advances in chemotherapy during the last 10 years include the development of new drugs for the prevention and treatment of side effects.
Hormone therapy for uterine cancer is used to slow the growth of grade 1 or 2 tumors uterine adenocarcinomas. The use of aromatase inhibitors will reduce the amount of the hormone estrogen in a woman's body by stopping tissues other than the ovaries from producing it.
Targeted therapy for uterine cancer targets the cancer’s specific genes, proteins, or the tissue environment to block cancer cell growth and spread while limiting damage to healthy cells.
Immunotherapy for uterine cancer is designed to boost the body's natural defenses to fight the cancer. Immunotherapy is approved by the US-FDA for uterine cancers with DNA mismatch repair defect or high microsatellite instability. PD-1 normally helps keep T cells from attacking other cells in the body (including some cancer cells). By blocking PD-1, these drugs boost the immune response against cancer cells. This can shrink some tumors or slow their growth.
The following factors may raise a woman’s risk of developing uterine cancer:
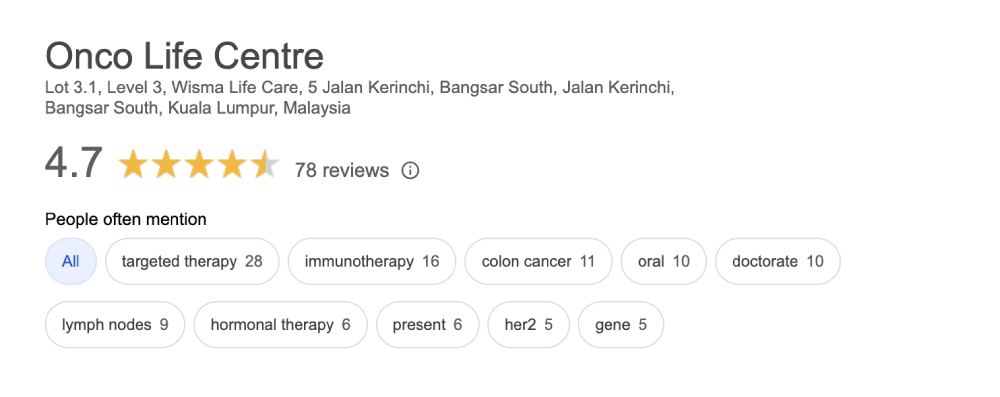
Onco Life Centre combines key elements of uterine cancer care and uterine cancer treatment under one roof, with convenience and speed. At Onco Life Centre, we have the necessary medical disciplines to achieve this. Our board certified highly experienced consultant oncologists have earned recognition for excellence in the field of uterine cancer treatment, providing our patients with the most advanced uterine cancer treatment options.

Dr. Christina Ng is a Consultant Medical Oncologist and Founder President of Empowered, The Cancer Advocacy Society of Malaysia.…
Treatment cost for uterine cancer depends on several factors, such as the staging and the type of the uterine cancer. Generally, using only chemotherapy is cheaper compared to using targeted therapy or immunotherapy. The more advanced the cancer stage, the more expensive it becomes to treat the cancer. At Onco Life Centre, the cost for treating uterine cancer using chemotherapy for most of our patients is around MYR6,000 per cycle. Adding in Targeted Therapy can go up from MYR8,000, depending on the specific type of targeted therapy drug used. The cost of uterine cancer immunotherapy can range from MYR10,000 and above depending on the specific type and dosage of immunotherapy drug used.
Patients and their families have opportunities to talk about the way they are feeling with our oncologists, nurses, counselors, or join our psychosocial program and support group at Onco Life Centre.