The pancreas is a pear-shaped gland located between the stomach and the spine. It is made up of 2 major components:
The exocrine component is made up of ducts and small sacs and makes enzymes that are released into the small intestine to help the body digest food, particularly fats.
The endocrine component is made up of islets of Langerhans and makes specific hormones like insulinoma, glucagonoma, somatostatin, pancreatic polypeptide (PP), and vasoactive intestinal peptide (VIP).




There are several types of pancreatic cancer, depending on whether the cancer began in the exocrine or endocrine component. Rarely, other types of cancer can begin in the pancreas, such as lymphoma and sarcoma.
Adenocarcinoma is the most common type of exocrine tumor. Rare types of exocrine pancreatic tumors include acinar cell carcinoma, adenosquamous carcinoma, colloid carcinoma, giant cell tumor, serous cyst adenoma, signetring cell carcinoma, squamous cell carcinoma and undifferentiated carcinoma.
These are also called pancreatic neuroendocrine tumors (PNETs) and make up 1% of pancreatic cancers. A PNET can be functioning or non-functioning. A functioning PNET is named based on the hormone produced such as insulinoma, glucagonoma and VIPomas.
Pancreatic cancer is treatable. In order to tailor your treatment plan, our pancreatic cancer oncologists at Onco Life Centre will review factors such as your pre-existing medical conditions, your overall health and nutritional status, as well as potential treatment side effects. When detected at an early stage, pancreatic cancer has a much higher chance of being successfully treated. However, there are also treatments that can help control the disease for patients with advanced stage pancreatic cancer to help them live longer.
Surgery for pancreatic cancer includes removing all or part of the pancreas,depending on the location and size of the tumor in the pancreas. A key goal of surgery is to have clear margins. Only about 20% of patients with pancreatic cancer are able to have surgery because most pancreatic cancers are first diagnosed when the disease has already spread. Surgery for pancreatic cancer may be combined with radiation therapy and/or chemotherapy, called adjuvant therapy. These treatments may sometimes be used before surgery to shrink a tumor. This is called neoadjuvant therapy.
External-beam radiation therapy is the type of radiation therapy used most often for pancreatic cancer. Chemotherapy may be given at the same time as radiation therapy because it can enhance the effects of the radiation therapy, which is called radio sensitization. Combining chemotherapy and radiation therapy may occasionally help shrink the tumor enough so it can be removed by surgery.
Chemotherapy is the use of drugs to destroy cancer cells, usually by stopping the cancer cells ability to grow and divide. A chemotherapy regimen usually consists of a specific number of cycles given over a set period of time. There is usually a rest period in between cycles. There are generally more side effects when 2 or more drugs are used together. Read More ...
Targeted therapy for pancreatic cancer is a treatment that targets the cancers specific genes, proteins or the tissue environment that contributes to cancer growth and survival. This type of treatment blocks the growth and spread of cancer cells while limiting damage to healthy cells. Read More ...
Immunotherapy drugs called checkpoint inhibitors can be used for patients whose pancreatic cancer cells have tested positive for specific gene changes, such as a high level of microsatellite instability (MSI-H), or changes in one of the mismatch repair (MMR) genes. Read More ...
Removal of the tumor and nearby lymph nodes if there are no signs that the disease has grown beyond the pancreas or spread to other parts of the body.
Chemotherapy, with or without radiation, to try to shrink the tumor and increase the chance of curative surgery.
Adjuvant chemotherapy usually starts within 8 weeks after surgery, based on how quickly a patient recovers. The option to use radiation therapy after surgery.
Chemotherapy with a combination of drugs can be used depending on each patients situation and overall health. Radiation therapy may be used, most often after chemotherapy if the cancer has not spread beyond the pancreas.
If the disease worsens during or after first-line treatment, options may include a different line of chemotherapy.
If cancer spreads to another part in the body from where it started, doctors call it metastatic cancer. Your treatment plan may include a combination of the treatments discussed above. Talk to our oncologists about your first and second line treatment options, which can heavily depend on your overall health and preferences.
Palliative care will also be important to help relieve symptoms and side effects. For most patients, a diagnosis of metastatic cancer is very stressful and, at times, difficult to bear. Patients and their families have opportunities to talk about the way they are feeling with our oncologists, nurses, counselors, or join our psychosocial program and support group.
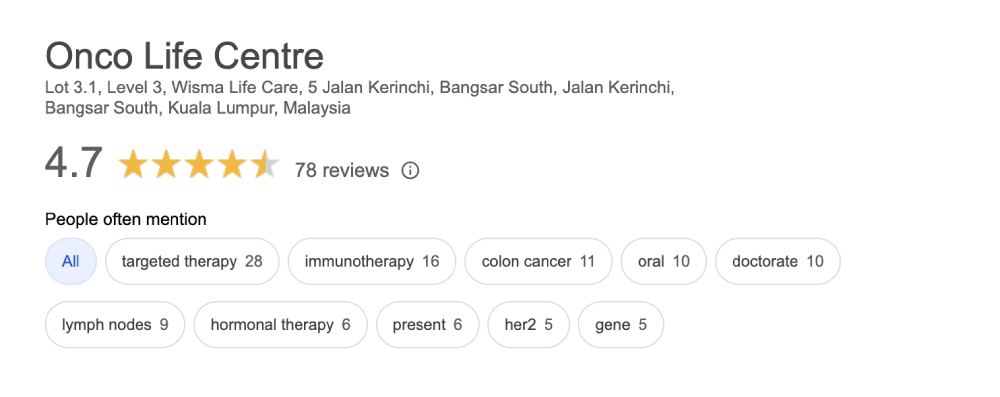
Onco Life Centre combines key elements of pancreatic cancer care and pancreatic cancer treatment under one roof, with convenience and speed. At Onco Life Centre, we have the necessary medical disciplines to achieve this. Our board certified highly experienced consultant oncologists have earned recognition for excellence in the field of pancreatic cancer treatment, providing our patients with the most advanced pancreatic cancer treatment options.

Dr. Christina Ng is a Consultant Medical Oncologist and Founder President of Empowered, The Cancer Advocacy Society of Malaysia.…
Treatment cost for pancreatic cancer depends on several factors, such as the staging and the subtype of the pancreatic cancer. Generally, using only chemotherapy is cheaper compared to using targeted therapy or immunotherapy. The more advanced the cancer stage, the more expensive it becomes to treat the cancer. At Onco Life Centre, the cost for treating pancreatic cancer using chemotherapy for most of our patients is around MYR4,000 per cycle. Adding in Targeted Therapy can go up from MYR6,000, depending on the specific type of targeted therapy drug used. Immunotherapy can range from MYR10,000 and above depending on the specific type and dosage of immunotherapy drug used.
Patients and their families have opportunities to talk about the way they are feeling with our oncologists, nurses, counselors, or join our psychosocial program and support group at Onco Life Centre.