Cancer of the esophagus begins in the inner layer of the esophageal wall and spreads through the esophageal wall, to lymph nodes as well as the blood vessels. Esophageal cancer can also spread to the lungs, liver, stomach, and other parts of the body.




There are 2 main types of esophageal cancer:
Squamous cell carcinoma of esophagus starts in the squamous cells that line the esophagus. It usually develops in the upper and middle part of the esophagus.
Adenocarcinoma of esophagus begins in the glandular tissue in the lower part of the esophagus, which leads to stomach.
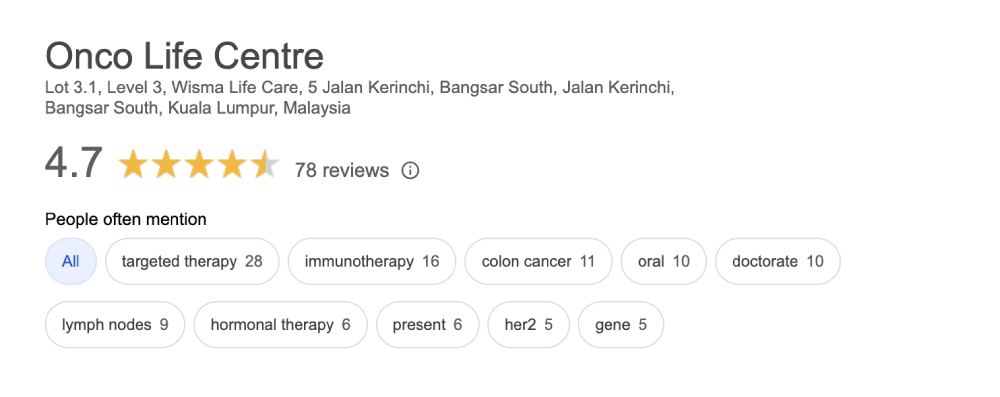
Treatment recommendations by our cancer specialists at Onco Life Centre are tailored, personalized and depends on tumor stage, tumor genomics (HER2, PDL1, TMB, MSI, NTRK1-3 fusion, BRAF, BRCA1, BRCA2, PALB2 gene mutation status), pre-existing medical conditions, your overall health and nutritional status.
Targeted therapy and immunotherapy is the foundation of precision medicine. Our Oncologists at Onco Life Centre work in close collaboration with Cancer Genomics Experts in the US to perform cancer gene mapping and DNA sequencing on our patients’ cancer tissue. Regular teleconferencing and live exchange of information with the US Genomics Experts allows our Oncologists to specifically design unique treatment plans for our patients. By targeting specific genes and proteins that are involved in driving cancer survival and progression, our patients at Onco Life Centre are experiencing significant and sustained improvements in their cancer responses and living longer.
At Onco Life Centre, we have made it our mission to improve the everyday lives of our patients. Our Oncologists and Pharmacists will seek to identify Compassionate Drug Access Programs that allows pre-approved new drugs outside clinical trials (and prior to product launch) for our patients who do not have satisfactory therapy options available.
For most people with locally advanced esophageal cancer, ASCO recommends chemo radiotherapy or chemotherapy before surgery because combined therapy has been shown to help people live longer. After chemo radiotherapy and surgery. Immunotherapy may be recommended if tumor cells are still found in the tissue removed during surgery. If surgery is not possible, the best treatment option is often a combination of chemotherapy and radiation therapy. Read More ...
Targeted therapy targets the cancer’s specific genes, proteins, or the tissue environment that contributes to cancer growth and survival. This type of treatment blocks the growth and spread of cancer cells while limiting damage to healthy cells. To find the most effective treatment, our oncologist will run tests to identify the genes, proteins, and other factors in your tumor. Read More ...
Immunotherapy is designed to boost your body's natural defenses to fight the cancer. The PD-1 pathway is critical in the immune system’s ability to control cancer growth. PD-1 and PD-L1 antibodies, which are called immune checkpoint inhibitors, block this pathway and can stop the growth of esophageal cancer. Drugs that target this pathway can be effective against MSI high or MSI-H, or PD-L1 positive esophageal cancers. Read More ...
Chemotherapy can be given before surgery to shrink the tumor and make it easier to completely remove it. Chemo may also be given, often along with radiation, after surgery to kill any groups of cancer cells that may have been left behind but are too small to be seen. The goal is to keep the cancer from coming back. Read More ...
Before surgery, radiation can be used along with chemo to try to shrink some tumors to make surgery easier. After surgery, radiation can be used to kill very small areas of cancer that cannot be seen and removed during surgery. Radiation, especially when combined with chemotherapy (chemo), might delay or prevent the cancer from coming back after surgery and may help people to live longer. Radiation can also be used to slow the growth and ease symptoms of advanced esophageal cancer such as pain, bleeding, and trouble eating.
Patients and their families have opportunities to talk about the way they are feeling with our oncologists, nurses, counselors, or join our psychosocial program and support group at Onco Life Centre.