Colorectal cancer or colon cancer, most often begins as a polyp and recognizing and removing precancerous polyps can prevent colorectal cancer. Colon polyps are commonly removed by performing polypectomy during colonoscopy. Most colorectal cancers are called adenocarcinoma. Other types of cancer that occur far less often in the colon or rectum include carcinoid tumor, gastrointestinal stromal tumor (GIST), small cell carcinoma, and lymphoma.
Most colorectal cancers (about 95%) are considered sporadic, meaning the genetic changes develop by chance after a person is born, so there is no risk of passing these genetic mutations on to ones children. Inherited colorectal cancers are less common (about 5%) and occur when genetic mutations are passed down from 1 generation to the next (see “family history of colorectal cancer” below).
Talk to our oncologists at Onco Life Centre about when screening should begin based on your age and family history of the disease. Using the guidelines below, you should begin colorectal cancer screening earlier and more often if you have any of the following risk factors:
In order to come up with the best treatment for colorectal cancer, our oncologists at Onco Life Centre will review factors such as your pre-existing medical conditions, your overall health and nutritional status, and potential treatment side effects. Treatment options and treatment plans for colorectal cancer follow the recommendations by our colon cancer specialists at Onco Life Centre based on the global NCCN and FDA guidelines.
Surgical resection is the removal of the tumor, some surrounding healthy tissue and nearby lymph nodes. Some patients may be able to have laparoscopic colorectal cancer surgery. The incisions are smaller and the recovery time is often shorter than with standard colon surgery. Laparoscopic surgery is as effective as conventional colon surgery in removing the cancer. Less often, a person with rectal cancer may need to have a colostomy. Sometimes, the colostomy is only temporary to allow the rectum to heal, but it may be permanent. With modern surgical techniques and the use of chemo-radiation before surgery, most people who receive treatment for rectal cancer do not need a permanent colostomy.
For rectal cancer, radiation therapy may be used before surgery, called neo-adjuvant therapy, to shrink the tumor so that it is easier to remove. It may also be used after surgery to destroy any remaining cancer cells. Chemotherapy is often given at the same time as radiation therapy, called chemo-radiotherapy, to increase the effectiveness of the radiation therapy. Chemo-radiation therapy is often used in rectal cancer before surgery to avoid colostomy or reduce the chance that the cancer will recur.
Chemotherapy for colorectal cancer destroys cancer cells, usually by stopping the cancer cells ability to grow and divide. Chemotherapy may be given after surgery to eliminate any remaining cancer cells. For some people with rectal cancer, chemotherapy is given with radiation therapy before surgery to reduce the size of a rectal tumor and reduce the chance of the cancer returning. Chemotherapy can be used in combination with Targeted Therapy to treat Stage 4 colorectal cancer.
Targeted therapy is a treatment that targets the cancers specific genes, proteins, or the tissue environment that contributes to cancer growth and survival. This type of treatment blocks the growth and spread of cancer cells while limiting damage to healthy cells. To find the most effective treatment, our oncologists at Onco Life Centre may run tumor profiling tests to identify the genes, proteins, and other factors in your tumor.
Anti-angiogenesis therapy is a type of targeted therapy that is focused on stopping angiogenesis, which is the process of making new blood vessels. Because a tumor needs the nutrients delivered by blood vessels to grow and spread, the goal of anti-angiogenesis therapies is to starve the tumor. In 2004, the FDA approved the first anti-angiogenesis monoclonal antibody along with chemotherapy as first-line treatment, for advanced colorectal cancer. An oral anti-angiogenesis tyrosine kinase inhibitor was approved in 2012 for patients with metastatic or Stage 4 colorectal cancer who have already received certain types of chemotherapy and other targeted therapies. Subsequently, newer anti-angiogenesis monoclonal antibodies combined with chemotherapy in the second-line setting for metastatic or Stage 4 colorectal cancer, were approved by the US FDA.
Epidermal growth factor receptor (EGFR) inhibitors are a type of targeted therapy that stop or slow down the growth of colorectal cancer. Currently, two FDA approved EGFR monoclonal antibodies are recommended for use only in patients with tumors that express non-mutated, or wild type, RAS genes. Our oncologists at Onco Life Centre may test your tumor for other molecular markers, including BRAF, microsatellite instability, and others.
The role of immunotherapy for advanced colon cancer treatment has been promising. Using immuntherapy in patients with mismatch-repair-deficient mutations or microsatellite instability in their tumors has shown remarkable results. An immunue-checkpoint inhibitor can be used on its own, or in combination with CTLA4 inhibitor for such patients.
In general, stages 0, 1, 2 and 3 colorectal cancer are often curable with surgery. However, many patients with stage 3 colorectal cancer, and some with stage 2, receive chemotherapy after surgery to increase the chance of eliminating the disease. Patients with stage 2 and 3 rectal cancer will also receive radiation therapy with chemotherapy either before or after surgery.
The usual treatment is a polypectomy, or removal of a polyp, during a colonoscopy.
The usual treatment is a polypectomy, or removal of a polyp, during a colonoscopy.
Surgery is often the first treatment. Patients with stage 2 colorectal cancer can talk to our oncologists at Onco Life Centre about whether adjuvant chemotherapy is needed after surgery to destroy any remaining cancer cells. For patients with stage 2 rectal cancer, radiation therapy is usually given in combination with chemotherapy, either before or after surgery.
Treatment for stage 3 colon cancer usually involves surgical removal of the tumor followed by adjuvant chemotherapy. For patients with rectal cancer, radiation therapy may be used along with chemotherapy before or after surgery, along with adjuvant chemotherapy.
Colorectal cancer can spread to distant organs, such as the liver, lungs, the tissue called the peritoneum that lines the abdomen, or a woman’s ovaries. Our oncologists at Onco Life Centre will help you tailor your treatment plan, which may include a combination of surgery, radiotherapy, targeted therapy, immunotherapy and chemotherapy. If the colorectal cancer has spread only to the liver (colorectal cancer liver metastasis) and if surgery is possible either before or after chemotherapy, there is a chance of complete cure. Even when curing the cancer is not possible, surgery may add months or even years to a person’s life. Determining who can benefit from surgery for cancer that has spread to the liver is often a complicated process that involves doctors of multiple specialties working together to plan the best treatment option. The role of immunotherapy for advanced colon cancer treatment has been promising. Using immuntherapy in patients with mismatch-repair-deficient mutations or microsatellite instability in their tumors has shown remarkable results. An immunue-checkpoint inhibitor can be used on its own, or in combination with CTLA4 inhibitor for such patients.
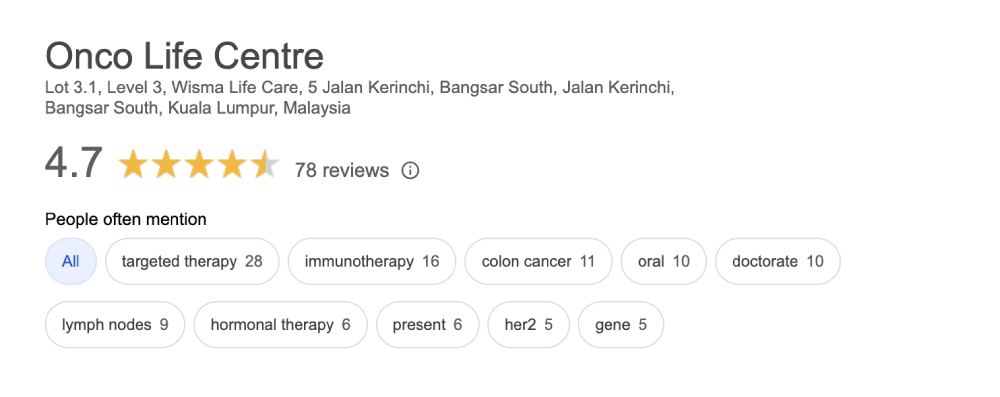
Onco Life Centre combines key elements of colorectal cancer care and colorectal cancer treatment under one roof, with convenience and speed. At Onco Life Centre, we have the necessary medical disciplines to achieve this. Our board certified highly experienced consultant oncologists have earned recognition for excellence in the field of colorectal cancer treatment, providing our patients with the most advanced colorectal cancer treatment options.

Dr. Christina Ng is a Consultant Medical Oncologist and Founder President of Empowered, The Cancer Advocacy Society of Malaysia.…
Treatment cost for colorectal cancer depends on several factors, such as the staging and also the sub-type of the colorectal cancer. Generally, using only chemotherapy is cheaper compared to using targeted therapy or immunotherapy. The more advanced the cancer stage, the more expensive it becomes to treat the cancer. At Onco Life Centre, the cost for treating colorectal cancer using chemotherapy for most of our patients is around MYR4,000 per cycle. Adding in Targeted Therapy can go up to MYR9,000, depending on the specific type of targeted therapy drug used. Immunotherapy can range from MYR10,000 and above depending on the specific type and dosage of immunotherapy drug used.
Patients and their families have opportunities to talk about the way they are feeling with our oncologists, nurses, counselors, or join our psychosocial program and support group at Onco Life Centre.