There are 2 main types of cervical cancer according to the cell origin of the cancer. Other types of cervical cancer are rare.
Squamous cell carcinoma makes up about 80% of all cervical cancers and start in the cells on the outer surface covering of the cervix.
Adenocarcinoma makes up 20% of all cervical cancer and start in the glandular cells that line the lower birth canal.




Cervical cancer can be prevented through regular screening as well as by receiving the HPV vaccine. The HPV vaccine is approved by the U.S. Food and Drug Administration (FDA) for prevention of cervical cancer caused by HPV for people between 9 and 45 years old.
Additional actions people can take to help prevent cervical cancer include:
Different organizations have looked at the scientific evidence, risks, and benefits of cervical cancer screening. The American Society of Clinical Oncology recommends that all women receive at least 1 HPV test to screen for cervical cancer in their lifetime.
Ideally, women 25 to 65 years old should receive an HPV test once every 5 years. Women 65 and older or who had a hysterectomy may stop screening if their HPV test results have been mostly negative over the previous 15 years.
The signs or symptoms of cervical cancer are:
The following tests may be used to diagnose cervical cancer:
Pap Smear & HPV typing test
A HPV test is done on a sample of cells from the patient’s cervix. HPV can be tested at the same time as a Pap test or after Pap test results show abnormal changes to the cervix. HPV16 and18 are seen more often in women with cervical cancer and may help confirm a diagnosis.
Colposcopy
The colposcope magnifies the cells of the cervix and vagina, similar to a microscope. It gives the doctor a lighted, magnified view of the tissues of the vagina and the cervix.
Biopsy
A biopsy is the removal of a small amount of tissue for examination under a microscope and enables a definite diagnosis to be made.
Computed tomography (CT) scan
A CT scan combines the pictures of the inside of your body into a detailed, 3-dimensional image that shows the tumor.
Magnetic resonance imaging (MRI)
An MRI uses magnetic fields to produce detailed images of the body and can be used to measure the tumor’s size.
Positron emission tomography (PET) scan
A small amount of a radioactive sugar substance is injected into the patient’s body. Cells that use the most energy take up this sugar substance. Because cancer tends to use energy actively, it absorbs more of the radioactive substance. A scanner then detects this substance to produce images of the inside of the body.
Staging is based on results of a physical exam, imaging scans, and biopsies.
The cancer has spread from the cervix lining into the deeper tissue but is still confined in the cervix.
The cancer has spread beyond the uterus to nearby areas, but it is still inside the pelvic area.
- Stage 2a cervical cancer
The tumor is limited to the upper two-thirds of the vagina and has not spread to the parametrial area.
- Stage 2b cervical cancer
The tumor has spread to the parametrial area but has not reached the pelvic wall.
The tumor has involved the lower third of the vagina, and has spread to the pelvic wall, and/or involving kidney and regional lymph nodes.
- Stage 4a cervical cancer
The cancer has spread to the bladder or rectum, but it has not spread to distant parts of the body.
- Stage 4b cervical cancer
The cancer has spread to distant parts of the body.
Treatment recommendations by our cervical cancer specialists at Onco Life Centre are tailored and depends on several factors, including the type and stage of cancer, possible side effects, the woman’s preferences and concerns about fertility and overall health.
For cervical cancer that has not spread beyond the cervix, these procedures are often used:
Radical hysterectomy is the removal of the uterus, cervix, upper vagina, and the tissue around the cervix and extensive pelvic lymph node dissection.
Bilateral salpingo-oophorectomy or removal of both fallopian tubes and both ovaries is often done.
Exenteration is the removal of the uterus, vagina, lower colon, rectum, or bladder if cervical cancer has spread to these organs after radiation therapy. Exenteration is rarely required.
The most common type of radiation treatment is called external-beam radiation therapy. When radiation treatment is given using implants, it is called brachytherapy. This combined approach is the most effective to reduce the chances the cancer will come back. Read More ...
The types of systemic therapies include:
1) Chemotherapy for cervical cancer
Chemotherapy is the use of drugs to destroy cancer cells, usually by keeping the cancer cells from growing, dividing, and making more cells. A chemotherapy regimen, or schedule, usually consists of a specific number of cycles given over a set period of time.
2) Targeted therapy for cervical cancer
Targeted therapy is a treatment that targets the cancer’s specific genes, proteins, or the tissue environment that contributes to cancer growth and survival. This type of treatment blocks the growth and spread of cancer cells while limiting damage to healthy cells. Not all tumors have the same targets. Read More ...
3) Immunotherapy for cervical cancer
Immunotherapy is designed to boost the body's natural defenses to fight the cancer. The PD-1 pathway is critical in the immune system’s ability to control cancer growth. Some cancer cells express the PD-L1 protein, which binds to the PD-1 protein on T cells. T cells are immune system cells that kill certain cells, like cancer cells. When the PD-1 and PD-L1 proteins bind, the T cell does not attack the cancer cell.
Immune checkpoint inhibitors are PD-1 inhibitor and block the binding between PD-1 and PD-L1, which allows the T cells to find and attack the cancer cells. Immune checkpoint inhibitors can be used to treat recurrent or metastatic cervical cancer.
The following factors may raise a woman's risk of developing cervical cancer:
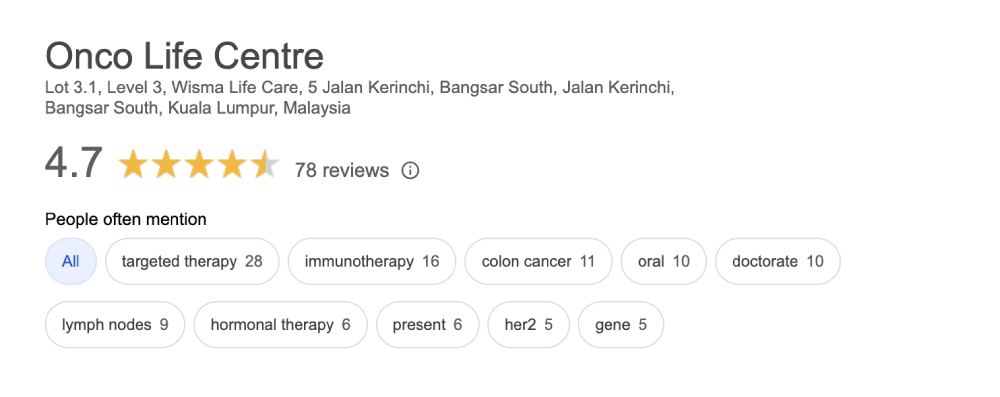
Onco Life Centre combines key elements of cervical cancer care and cervical cancer treatment under one roof, with convenience and speed. At Onco Life Centre, we have the necessary medical disciplines to achieve this. Our board certified highly experienced consultant oncologists have earned recognition for excellence in the field of cervical cancer treatment, providing our patients with the most advanced cervical cancer treatment options.

Dr. Christina Ng is a Consultant Medical Oncologist and Founder President of Empowered, The Cancer Advocacy Society of Malaysia.…
Treatment cost for cervical cancer depends on several factors, such as the staging of the cervical cancer. Generally, using only chemotherapy is cheaper compared to using targeted therapy or immunotherapy. The more advanced the cancer stage, the more expensive it becomes to treat the cancer. At Onco Life Centre, the cost for treating cervical cancer using chemotherapy for most of our patients is around MYR6,000 per cycle. Adding in Targeted Therapy can go up from MYR8,000, depending on the specific type of targeted therapy drug used. Cost of immunotherapy for cervical cancer can range from MYR10,000 and above depending on the specific type and dosage of immunotherapy drug used.
Patients and their families have opportunities to talk about the way they are feeling with our oncologists, nurses, counselors, or join our psychosocial program and support group at Onco Life Centre.