Treatment options and treatment plans for early breast cancer and metastatic breast cancer follow the recommendations by our breast cancer specialists at Onco Life Centre based on the global NCCN and FDA guidelines. The best way to treat breast cancer, or even to cure breast cancer, depends on several factors such as stage of the tumor, tumor’s subtype (ER, PR, HER2, PDL1 and PIK3CA gene mutation status), genomic markers, patient’s age, patient’s menopausal status, the presence of BRCA1 or BRCA2 mutations. Along with staging investigations, other tools can help estimate prognosis and help our specialists make decisions about adjuvant therapy. Onco Life Centre arranges tumor profiling tests at renowned genomics and genetic laboratories in the USA and Europe, which can determine the most optimum type of treatment protocol with the maximum benefits.

For both DCIS and early-stage breast cancer, surgery is recommended to remove the tumor. Women with a very high risk of developing a new cancer in the other breast may consider a bilateral mastectomy. This includes women with BRCA1 or BRCA2 gene mutations and women with cancer in both breasts. Read More ...

The most common type of radiation treatment for breast cancer is called external-beam radiation therapy. Most commonly, radiation therapy is given after a lumpectomy, and following adjuvant chemotherapy if recommended. This helps lower the risk of cancer recurrence in the breast. In fact, with modern surgery and radiation therapy, recurrence rates in breast cancer are now less than 5%. Read More ...

Chemotherapy can be used to treat Stage 1, Stage 2, Stage 3 and Stage 4 breast cancer. Chemotherapy destroys cancer cells by stopping the cancer cells’ ability to grow and divide. Chemotherapy may be given before surgery to shrink a large tumor (neo-adjuvant chemotherapy). It may also be given after surgery to reduce the risk of recurrence (adjuvant chemotherapy). Chemotherapy is also given for metastatic breast cancer. There are many different types of chemotherapy schedules. Research has shown that combinations of certain drugs are sometimes more effective than single drugs for adjuvant treatment. The number of chemotherapy cycles will depend on the chosen treatment protocol.

Hormonal therapy is an effective treatment for ER and PR expressing tumors in both early-stage and metastatic breast cancer. Blocking the hormones can help prevent a cancer recurrence and death from breast cancer when used for early-stage disease. Hormone therapy for breast cancer shrinks the cancer and improves cancer-related symptoms in metastatic breast cancer. Read More ...

Targeted therapy for breast cancer targets the cancer’s specific genes, proteins, or the tissue environment that contributes to cancer growth and survival. Anti HER2 monoclonal antibody treatment is approved for both adjuvant therapy and advanced HER2-positive breast cancer. A combination of two different types of monoclonal antibody and chemotherapy improves the treatment effectiveness, and lengthen lives in the first-line setting. Additionally, there are other second-line approved anti HER2 options available for the treatment of metastatic breast cancer after failure of first-line treatment. Read More ...

Immunotherapy for breast cancer is designed to boost the body's natural defenses to fight the cancer. In 2019, the U.S. Food and Drug Administration (FDA) approved a combination of Immune checkpoint inhibitor and a plus-protein-bound chemotherapy drug for advanced PD-L1 expressing triple-negative breast cancer. Read More ...

Bisphosphonates are drugs that block the cells that destroy bone, called osteoclasts. Bisphosphonates can be used for bone metastasis. Research suggests that it may reduce breast cancer recurrences, particularly in bone, when given in postmenopausal women. Read More ...
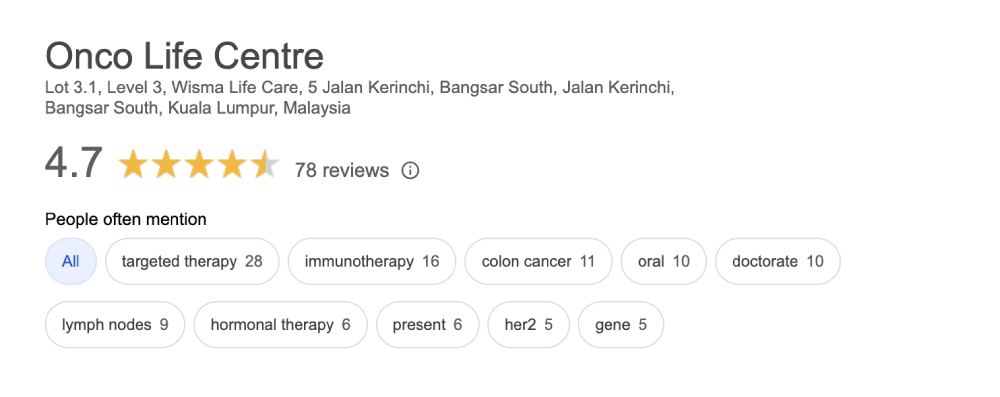
Onco Life Centre combines key elements of breast cancer care and breast cancer treatment under one roof, with convenience and speed. At Onco Life Centre, we have the necessary medical disciplines to achieve this. Our board certified highly experienced consultant oncologists have earned recognition for excellence in the field of breast cancer treatment, providing our patients with the most advanced breast cancer treatment options.

Dr. Christina Ng is a Consultant Medical Oncologist and Founder President of Empowered, The Cancer Advocacy Society of Malaysia.…
Treatment cost for breast cancer depends on several factors, such as the staging and also the sub-type of the breast cancer. Generally, using only chemotherapy is cheaper compared to using targeted therapy or immunotherapy. The more advanced the cancer stage, the more expensive it becomes to treat the cancer. At Onco Life Centre, the cost for treating breast cancer using chemotherapy for most of our patients range from MYR4,000 to MYR6,000 per cycle. Using Targeted Therapy can range from MYR4,000 and above, depending on the specific type of targeted therapy drug used. Immunotherapy can range from MYR8,000 and above depending on the specific type and dosage of immunotherapy drug used.
Patients and their families have opportunities to talk about the way they are feeling with our oncologists, nurses, counselors, or join our psychosocial program and support group at Onco Life Centre.